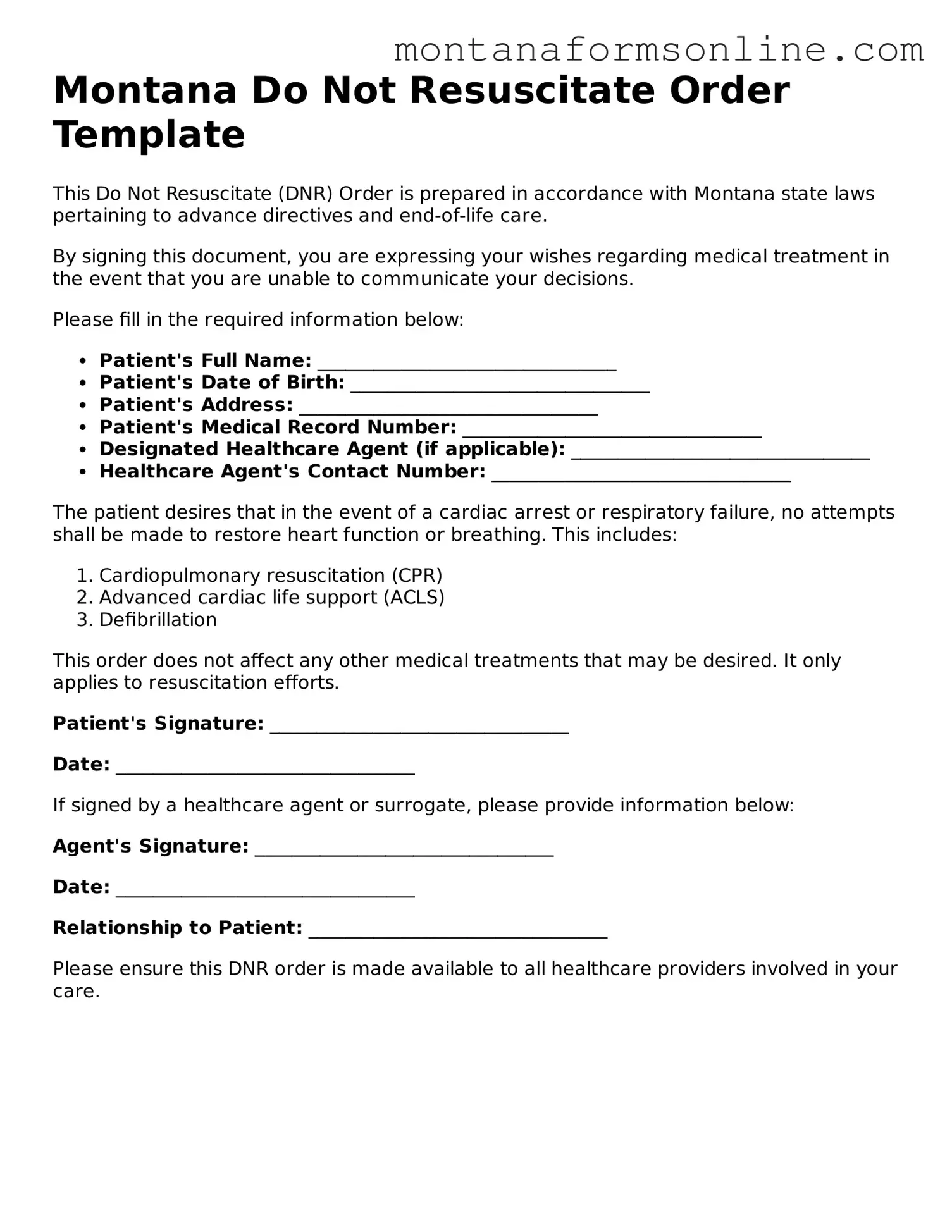
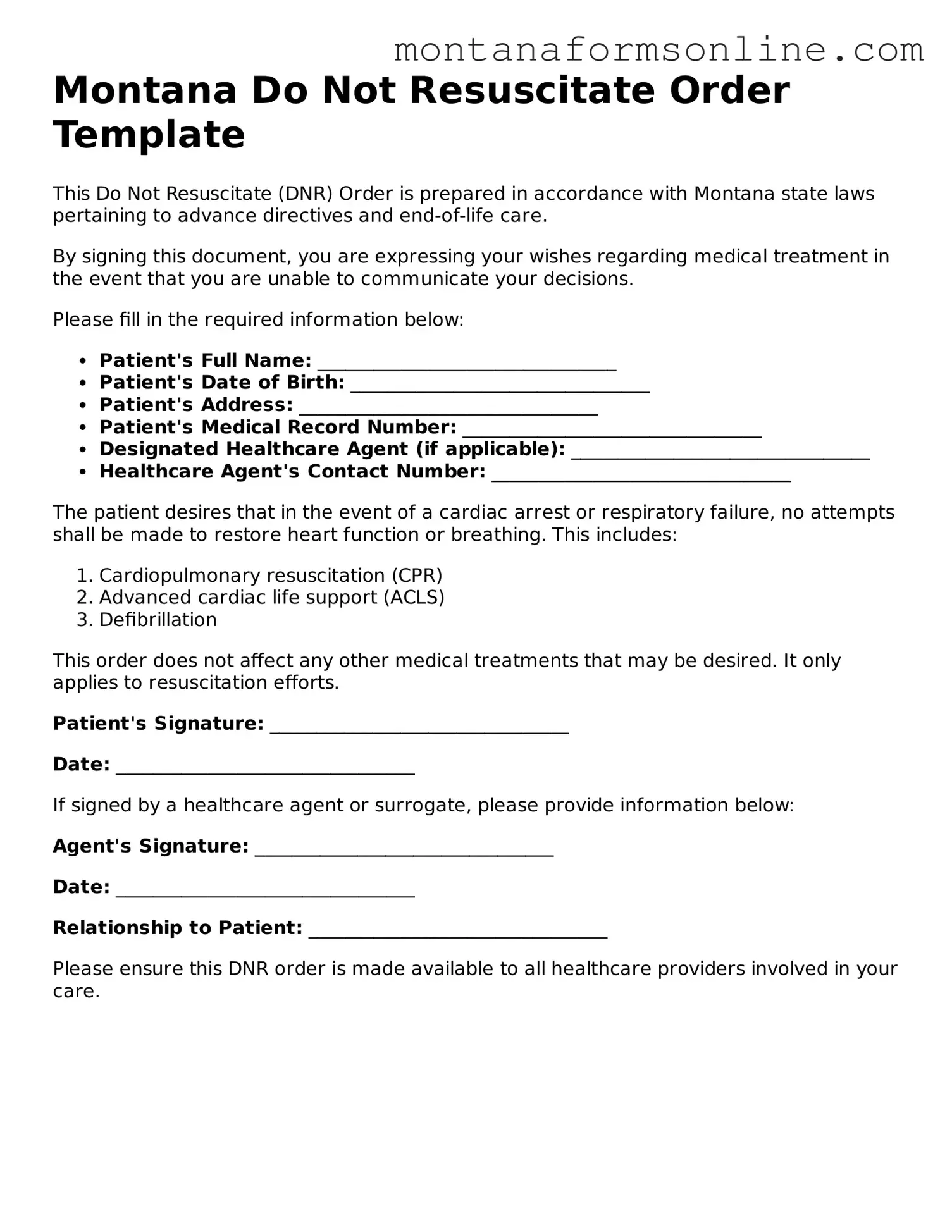
The Montana Do Not Resuscitate (DNR) Order form shares similarities with the Advance Directive. An Advance Directive is a legal document that outlines a person's preferences regarding medical treatment in the event they become unable to communicate their wishes. Both documents aim to ensure that a patient's healthcare choices are respected, allowing individuals to express their desires about life-sustaining measures. While the DNR specifically addresses resuscitation efforts, the Advance Directive covers a broader range of medical decisions, including the use of ventilators and feeding tubes.
The IRS 2553 form is an important document for small businesses, much like how various medical directives ensure one's healthcare preferences are respected. It allows eligible corporations to elect S corporation status for tax purposes, functioning as a means for entities to be taxed as pass-through entities. This can lead to significant tax savings for businesses. Understanding how to correctly file Form 2553 is as crucial as comprehending the implications of a DNR order or living will. For those seeking guidance on tax matters related to Form 2553, valuable resources are available, such as smarttemplates.net.
Another document akin to the Montana DNR is the Physician Orders for Life-Sustaining Treatment (POLST). The POLST form is designed for individuals with serious illnesses or those who are nearing the end of life. Like the DNR, the POLST communicates a patient’s preferences regarding resuscitation and other life-sustaining treatments. It serves as a medical order, ensuring that healthcare providers follow the patient's wishes in emergencies. Both documents are intended to facilitate discussions between patients, families, and healthcare providers about end-of-life care.
The Medical Power of Attorney (MPOA) is also similar to the DNR Order. An MPOA allows individuals to appoint someone to make medical decisions on their behalf if they are unable to do so. While the DNR focuses specifically on resuscitation, the MPOA encompasses a wider range of healthcare decisions. Both documents empower individuals to maintain control over their medical care and ensure that their preferences are honored, even when they cannot voice them directly.
The Living Will is another document that shares common ground with the Montana DNR. A Living Will is a written statement that outlines a person’s wishes regarding medical treatment in situations where they cannot express their preferences. Similar to the DNR, it addresses the types of medical interventions an individual does or does not want. The key difference lies in the Living Will's broader scope, which may include preferences about pain management and other life-sustaining treatments beyond resuscitation.
The Do Not Intubate (DNI) order is closely related to the DNR. A DNI specifically instructs healthcare providers not to place a patient on a ventilator if they are unable to breathe on their own. While the DNR focuses solely on resuscitation efforts, the DNI addresses a particular aspect of respiratory support. Both documents reflect a patient’s wishes regarding critical medical interventions, ensuring that their preferences are respected during emergencies.
The Comfort Care Order is another document that aligns with the Montana DNR. This order focuses on providing comfort to patients rather than prolonging life through aggressive treatments. It emphasizes palliative care, which prioritizes quality of life and symptom management. While the DNR may indicate a refusal of resuscitation, the Comfort Care Order goes further by outlining a patient’s desire for minimal medical intervention, ensuring a peaceful and dignified end-of-life experience.
The Hospice Care Plan is similar in that it outlines the goals and preferences for care at the end of life. Hospice care focuses on providing comfort and support for patients with terminal illnesses. While the DNR specifically addresses resuscitation, the Hospice Care Plan encompasses a comprehensive approach to managing symptoms and improving the quality of life. Both documents emphasize the importance of honoring a patient's wishes and ensuring they receive the care they desire during their final days.
The Treatment Preferences form is another document that complements the DNR. This form allows individuals to specify their treatment preferences in various medical situations, including resuscitation. It serves as a guide for healthcare providers, ensuring that they understand the patient’s wishes. While the DNR is limited to resuscitation decisions, the Treatment Preferences form can cover a broader spectrum of medical interventions, making it a valuable tool in end-of-life planning.
Finally, the Health Care Proxy is similar to the DNR Order in that it designates an individual to make healthcare decisions on behalf of someone else. This document is particularly useful when a person is unable to communicate their wishes. While the DNR specifically addresses resuscitation, the Health Care Proxy allows the appointed individual to make a variety of medical decisions, ensuring that the patient’s overall care aligns with their values and preferences.